Lymph node metastasis from non-melanoma skin cancer
Abstract
The management of non-melanoma skin cancers metastatic to the neck is challenging due to variability in biological behavior and patterns of regional lymphatic spread. Metastatic non-melanoma skin cancers to the parotid and neck often behave aggressively, with a high incidence of local recurrence after treatment and reduced five-year survival outcomes. Patterns of lymphatic spread are different from those seen in mucosal squamous cell carcinoma, with higher prevalence of disease in the parotid and superficial lymphatics. These factors require that treatment is individualized to achieve optimal outcomes. Traditionally, the management of non-melanoma skin cancers metastatic to lymph nodes has involved surgical excision followed by adjuvant radiation therapy. However, novel systemic therapies are showing promising results and their role in the management of these cancers is evolving.
Keywords
INTRODUCTION
Patterns of spread
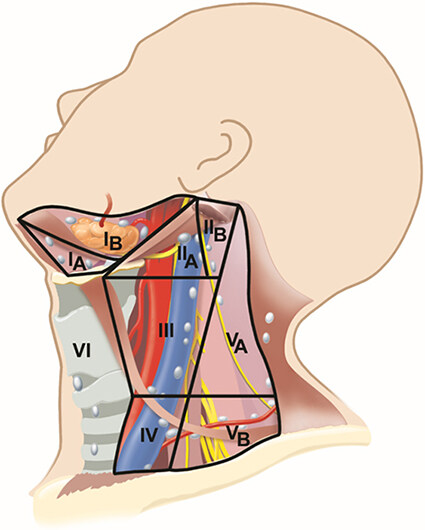
In contrast to mucosal origin malignancies which predominantly metastasize to lymph nodes in levels I-V in the neck (shown in Figure 1), cutaneous malignancies of the head and neck can also metastasize to the pre- and post-auricular, parotid, suboccipital, and superficial lymphatic systems, depending on tumor location.
Figure 1. Assigned lymph node levels of the lateral neck. Level IA: Submental nodes. Level IB: Submandibular nodes. Level IIA: Upper jugular nodes anterior to the spinal accessory nerve. Level IIB: Upper jugular nodes posterior to the spinal accessory nerve. Level III: Mid jugular nodes. Level IV: Lower jugular nodes. Level VA: Posterior triangle nodes superior to the level of the inferior border of cricoid cartilage. Level VB: Posterior triangle nodes inferior to the level of the inferior border of cricoid cartilage. Level VI: Central compartment nodes.
Patterns of lymphatic drainage are predictable based on the location of the primary tumor, shown in Figure 2. This information can be used to guide the management of regional diseases from specific primary sites[1]. As a general rule, a line joining the helix of one ear to the helix of the opposite ear in a coronal plane separates the watershed areas of the scalp. Tumors located anterior to this line generally metastasize to preauricular, periparotid, intraparotid, and anterior cervical lymph nodes (levels I-IV), whereas tumors of the scalp posterior to this line usually metastasize to the postauricular and suboccipital lymph nodes, as well as those in the posterior triangle of the neck and deep jugular chain[1]. For example, cutaneous malignancies on the cheek, eyelids, pinna, forehead, and temple have been reported as draining initially to preauricular, periparotid, and parotid nodes[2]. Most lymph nodes within the parotid are found superficial to the facial nerve, and these are typically involved in cutaneous malignancy; however, a small number of nodes can be present deep in the nerve[3,4].
RISK OF REGIONAL METASTASIS
Although non-melanoma skin cancer (NMSC) has a lower propensity for advanced disease than cutaneous melanoma, the absolute mortality burden has recently surpassed that of melanoma[5]. Cutaneous squamous cell carcinoma (SCC) and Merkel cell carcinoma (MCC) have the highest risk of metastasis to regional nodes[6,7]. Other NMSCs can also present with regional diseases in the parotid and neck, such as cutaneous adnexal tumors, cutaneous sarcomas and, rarely, basal cell carcinoma (BCC). The presence of lymph node disease is a poor prognostic factor in NMSC. For SCC, it has been suggested that the presence of nodal metastasis is a stronger predictor of prognosis than features present in the primary tumor[8].
Squamous cell carcinoma
Approximately 3.7%-5.8% of cases of cutaneous SCC present with regional disease[9-12]. However, higher rates of 33%-47% are reported in association with several clinical and histological features[13,14]. These include tumor location (ear, lip, or temple), size > 2 cm, depth of invasion > 6 mm or beyond subcutaneous fat, histologic type, degree of differentiation, perineural invasion, and immunosuppression[15-18]. Immunocompromise is a significant independent risk factor for the aggressive behavior of metastatic cutaneous SCC to the neck[19,20]. Presence of disease in regional nodes from cutaneous SCC has been associated with five-year survival rates ranging from 35%-70%, depending on tumor stage, surgery, and adjuvant treatment [14,16,21-25].
Merkel cell carcinoma
MCC is a neuroendocrine carcinoma with a high propensity for regional spread of over 50% and, even in cases without clinical evidence of lymph node metastasis, the rate of nodal micrometastasis on sentinel lymph node biopsy can be 30%-38%[26]. MCC of unknown primary occurs in 5%-25% of cases and carries improved survival and different tumor characteristics compared to tumors with presence of a primary[27-30]. Increasing nodal disease burden has been suggested as a prognosticator in MCC[31].
Basal cell carcinoma
While BCC is the most common primary cutaneous malignancy found in the head and neck[32], it rarely metastasizes to lymph nodes. Rates of nodal disease from primary BCC are reported between 0.0028% to 0.55%[33]. Regional spread from BCC is associated with male gender, fair skin, and history of radiation, as well as primary tumor factors such as increased size, deeper invasion, perineural invasion, basosquamous histology, and primary site in the head and neck[33-36].
Adnexal tumors
Cutaneous adnexal tumors, including those involving hair follicles, sweat ducts, ceruminous glands, sebaceous glands, apocrine glands, and eccrine glands, may occur sporadically or as part of genetic syndromes. Rates of regional spread are uncertain due to the rare and heterogeneous nature of these tumors; however, the presence of lymph node metastases portends significantly worse overall survival[37]. It has been suggested that these tumors are more likely to demonstrate nodal involvement with aggressive local histology, and that lymphatic disease in early-stage tumors is rare[38,39], but high rates of up to 89% have also been reported[40].
Cutaneous sarcoma
Regional lymph node metastasis is reported at up to 23% in angiosarcoma[41] and 10%-20% in pleomorphic dermal sarcoma[42]. However, other non-melanoma cutaneous malignancies of the head and neck, such as atypical fibroxanthoma, leiomyosarcoma, or dermatofibrosarcoma, rarely spread regionally, with rates less than 10% in most of these tumors[43].
CLINICAL ASSESSMENT
Clinical evaluation of the entire skin of the head and neck, including the scalp, must be performed to assess for multifocal lesions or in-transit metastatic disease. A thorough examination of the parotid and neck should be performed in all patients with cutaneous malignancy of the head and neck. In cases that present with clinical nodal disease, anatomical structures are particularly important to consider, including underlying cartilage, underlying bone, parotid gland, external auditory canal, temporomandibular joint, lateral temporal bone, motor nerves, such as the facial nerve branches, and cutaneous sensory nerves, such as the greater auricular and auriculotemporal nerves. For facial skin lesions, involvement of the nasal cartilages and tarsal plates for lesions of the eyelid, as well as the involvement of the terminal divisions of the trigeminal nerve, should be carefully assessed.
SCC has a significant propensity for perineural spread or direct nerve invasion by nodal disease, and so particular care must be taken to assess and manage sensory and motor nerves in these cases. Thorough clinical examination should also include the extent of involvement of the skin, particularly in morpheaform BCC and dermal lymphatic permeation by aggressive cancers.
Metachronous presentation of regional lymph node metastasis from NMSC is common and can be difficult to distinguish from primary mucosal site metastasis. In these cases, histological assessment, such as for high-risk human papillomavirus by in situ hybridization, can be helpful, and a thorough evaluation for a mucosal primary is critical.
For clinically suspected nodal disease, as well as for primary tumors with a high risk of nodal involvement, imaging should be performed to further evaluate the presence and extent of nodal metastases. This typically will include contrast-enhanced computed tomography (CT) scanning of the head, neck, and chest. CT scans are also valuable to assess bone invasion by primary tumors in extensive lesions. Magnetic resonance imaging (MRI) is valuable for the assessment of suspected perineural invasion or parapharyngeal involvement, while Positron emission tomography/CT imaging can be used in some cases for the assessment of distant metastases, in addition to ruling out a mucosal primary site in those with metachronous presentations. Ultrasound-guided fine-needle aspiration or core biopsy can be used to establish diagnosis.
STAGING
NMSC of the head and neck is staged according to the 8th edition of the American Joint Committee on Cancer (AJCC) tumor, node, metastasis (TNM) classification system[44]. For tumors involving the temporal bone, the most commonly used staging system is the modified University of Pittsburgh system[45].
There has been some debate around the use of the AJCC staging system in cutaneous SCC[46,47]. The nodal system is the same as for mucosal SCC, but it is likely that stratification does not adequately reflect the differences between nodal spread of mucosal and cutaneous SCC[48,49]. For example, very high rates of extranodal extension in cutaneous SCC means that nodes greater than 6 cm in size without extranodal extension are extremely rare and so the N3a stage may be better reclassified based on other features such as the number of nodal metastases[44,49]. It has been suggested that an increasing number of metastatic lymph nodes, separately from the presence of extranodal extension, is an independent predictor of disease-specific survival in cutaneous SCC of the head and neck and could be incorporated into AJCC staging[50-52]. However, alternative staging systems for regional spread of cutaneous SCC have been proposed, which may give better stratification[53]. These staging systems are often used for research purposes leading to inconsistency in the significance of parotid involvement in staging. Examples of commonly used staging systems include the Brigham and Women’s system[54], Clark’s N1S3 system[55], O’Brien’s parotid and neck node system[56], and the Immunosuppression, Treatment, Extranodal spread, and Margin status prognostic score[57].
For MCC, multiple staging systems have been described[58]; however, a distinct AJCC TNM staging system, separate from other NMSC, is now most commonly used. Any regional nodal involvement is classified as stage N1, while regional nodal involvement with in-transit metastasis is classified as stage N3. Stage N2 disease is classified by the presence of in-transit metastasis without nodal disease present. Overall, stage III disease is denoted by any primary tumor size or unknown primary, with regional lymph node involvement.
For cutaneous adnexal tumors of the head and neck, regional lymph node staging is important due to its impact on prognosis[37]. Staging, along with other NMSC, is according to the 8th edition AJCC system.
SURGICAL MANAGEMENT
Multiple guidelines exist to assist decision making in the management of NMSC. However, this can be a challenge as evidence from high-quality clinical trials is rare[59]. When possible, surgery remains the mainstay of management of this disease, including in cases of regional spread.
Squamous cell carcinoma
Reported rates of metastatic spread from the superficial parotid nodes to the cervical lymph nodes in SCC range from 13%-35%[56,60-62]. Moreover, since metachronous metastasis is common, some research has suggested elective treatment of the neck and parotid in advanced stage or high-risk cutaneous SCC[21,63-68]. However, no prospective study has demonstrated a clinically substantial survival benefit to elective neck dissection compared to therapeutic neck dissection after nodal metastasis has developed, and recent data reports worse overall survival in those undergoing elective neck dissection[69,70]. Elective treatment of the neck in regionally metastatic head and neck NMSC remains controversial and prospective trials are needed to clarify optimal management.
For clinically node-negative high-risk SCC, depending on their age, co-morbidities, and risk factors, sentinel lymph node biopsy or observation with or without imaging may be considered alternatives to elective neck dissection and parotidectomy[21,70,71]. Although sentinel lymph node biopsy is a viable tool in head and neck melanoma and is also used in MCC, it is rarely used in other head and neck cutaneous malignancies outside of clinical trials[72-74]. Issues with sentinel lymph node mapping in the head and neck include proximity of the injection site to the draining basins, unpredictable lymphatic drainage, multiple sentinel nodes per patient, higher risk of false-negative results, and mapping to the parotid gland in
Up to 75% of nodal metastases from cutaneous SCC of the head and neck are present in the parotid gland[76]. Typical management of this presentation, when resectable, is surgery followed by adjuvant radiation[77], because radiation alone for clinically positive disease is associated with worse survival outcomes[78]. For cases with involved cervical nodes, in which parotid nodes are not clinically present but the primary tumor site is associated with a high risk for parotid spread, either parotidectomy can be carried out alongside the neck dissection, or adjuvant radiation can be used to treat the parotid. It is also important to resect the external jugular lymphatics in these cases and level V for tumors based posteriorly[2,64,72,79].
For patients with parotid nodal metastases who are otherwise clinically node-negative, additional elective selective neck dissection would include levels I-III for anterior facial primaries, levels II-III for anterior scalp and external ear primaries, and levels II-V including postauricular and suboccipital nodes for posterior scalp and neck primaries[79].
Although it has been suggested that total parotidectomy be considered when positive parotid nodes are identified[69,80,81], there is potential for higher complications from this, and so it may only be beneficial in cases with definite deep lobe involvement[56,82,83]. Radical or extended radical parotidectomy may be necessary depending on the involvement of adjacent structures[81]. When metastatic cutaneous SCC is adherent to the temporal bone, some form of lateral temporal bone surgery should be carried out[84], which may be aggressive and require adjuvant radiation[85].
Trigeminal, facial and cervical plexus nerves can be at risk of cutaneous malignancy, usually by the primary tumor itself, but also potentially by regional nodal disease, particularly if extranodal extension is present[69,86]. This is usually due to direct invasion by nodal disease, but can also be due to perineural spread, and the parotid gland is more likely involved than the neck. The likelihood of nerve sacrifice is highest in patients with nodal disease within the body of the parotid gland and when the primary tumor itself demonstrates perineural invasion[87]. For patients with clinical perineural invasion, available evidence suggests that survival is improved by surgical resection if feasible, followed by postoperative radiation[88-91]. Facial nerve function is an important outcome for patients with cancer of the parotid and temporal bone region[92], and ideally, it should only be sacrificed when directly compromised by disease[69,82]. If oncologic resection is not possible without sacrificing the nerve, it may require partial or complete resection even if it is functioning preoperatively. For example, radical resection to ensure clear margins may be necessary for tumors at the stylomastoid foramen even when the nerve is clinically intact[84], but efforts should be made to preserve the nerve where possible. Intraoperative frozen section to ensure satisfactory clearance of perineural disease may potentially remove any individual effect on survival[85]. Parotid nodal disease may directly involve the auriculotemporal nerve or spread to it via anastomoses with the facial nerve, with subsequent spread to the infratemporal fossa and foramen ovale[93-95], in which case partial mandibular resection may be needed to access the infratemporal fossa.
Merkel cell carcinoma
Status of spread to the lymph nodes is the most important predictor of survival in MCC. Survival has been reported at 52% for MCC with metastasis to regional nodes, compared to 71% in cases without metastasis[96]. As micrometastasis is common, and independent of size or depth, sentinel lymph node biopsy is recommended for all patients with MCC and is included in the AJCC 8th edition staging system[97]. When disease is identified in sentinel nodes, lymph node dissection is suggested, although there are no prospective studies demonstrating its benefit, and so radiation may be an alternative[96,98].
Basal cell carcinoma
Regional lymph node metastasis from BCC is exceedingly rare but portends a poorer prognosis than localized disease[35]. Due to its rarity, no guidelines are established. However, treatment has typically been with therapeutic neck dissection and possible adjuvant radiation.
Adnexal tumors
For cutaneous adnexal tumors, lymph node metastases identified after sentinel lymph node biopsy in early-stage tumors are rare[38], so it may best be applied selectively, possibly only in patients with local recurrence[39]. One study suggested that apocrine carcinoma demonstrates high rates of lymphatic spread, and so elective node dissection should be considered in this histology, although no cases in this study were in the head and neck, in which regional spread may be less common[40,99].
RECONSTRUCTION
Large defects in the parotid and neck region after clearance of nodal metastases may require a pedicled or free flap[100], particularly in cases where adjuvant radiation is likely or good cosmesis is sought. However, adjuvant radiation can result in significant free flap volume loss and so overcorrection is sometimes required to ensure adequate function after radiation[101]. In cases where the primary tumor involves the skull base, closure is usually done in layers to prevent cerebrospinal fluid leak and close dead space[102].
For larger defects that include parotidectomy and neck dissection, an anterolateral thigh flap is typically employed[103]. Alternative local flaps to reconstruct the parotid region, for example, in cases where free tissue transfer may be contraindicated, include the temporalis muscle flap, supraclavicular island flap, scalp flap, preauricular flap, or temporoparietal fascia flap.
In cases with extensive perineural invasion, static facial reanimation can be used and this is sometimes incorporated into the flap of choice[102]. Dynamic reconstruction can be carried out using autologous nerve grafts such as the greater auricular or sural nerves, the latter of which can be used for multiple anastomoses. Nerve allografts can also be used for dynamic reconstruction, as well as masseteric or hypoglossal nerve transfers, with oral commissure symmetry better in hypoglossal nerve use and time to the first movement quicker in masseteric nerve use[104].
RADIATION
Radiation in regional lymph node metastases from NMSC is typically reserved for the adjuvant setting. However, for cases undergoing parotidectomy for parotid nodal disease, elective neck radiation can be an alternative to elective neck dissection with adjuvant radiation[105]. Radiation or chemoradiation as primary treatment can be considered in patients deemed unfit for surgical management[106].
For node-positive cases, adjuvant treatment is typically given to all patients with nodal disease greater than 3 cm with no extracapsular extension, those with extranodal extension, or those with incompletely excised nodal disease. Some evidence suggests that it may also be considered with one positive lymph node ≤ 3 cm with no extracapsular extension[107,108]. The recommended dose of adjuvant radiation is 60 Gy in 2.0 Gy once-daily fraction, 5 days per week, or a biologically equivalent dose[109]. Techniques such as Intensity-modulated radiation treatment (IMRT), or volumetric modulated arc therapy are preferable. Non-IMRT techniques, including 3-dimensional conformal radiation and electron or proton beam therapy, are acceptable if adequate tumor coverage is achieved while constraints on organs at risk are met[109]. Brachytherapy use is limited to previously irradiated patients with incompletely resectable nodal disease.
The role of concurrent chemotherapy with radiation is controversial and is less certain than in cases of mucosal SCC. Some research has suggested a lower chance of recurrence[110], but there has been no evidence to suggest improvement in overall survival by the addition of chemotherapy[23], and it is possible that outcomes could be worse with the use of concurrent chemotherapy[111]. Concurrent chemotherapy is typically used in cases of mucosal SCC demonstrating extranodal extension, and it has been associated with worse outcomes in cutaneous SCC, but this feature in cutaneous SCC is associated with higher nodal burden and may be different from the tumor biology associated with mucosal disease[50]. Thus, further research is needed to determine if there is any role for concurrent chemotherapy with radiation in the adjuvant setting for NMSC. Recent studies evaluating the use of radiotherapy with immunotherapy, such as cemiplimab or pembrolizumab, in locally advanced unresectable cutaneous SCC have shown promising results and further research is needed to clarify the role of concurrent radiation with immunotherapy[112-114].
Separately, MCC is a highly radiosensitive tumor. Treatment of the neck includes either elective nodal radiation[115,116], or sentinel node biopsy followed by adjuvant radiation or lymph node dissection if positive, or by observation alone if negative[116,117]. Elective nodal radiation may be avoided in T1 cases with negative sentinel nodes[118,119]. Conventionally fractionated radiation with a dose of 50 Gy in 25 fractions is used in the elective setting[120], however, single fraction treatment with 8 Gy has also been proposed[121]. For lymph node metastases, adjuvant radiation is advocated to improve locoregional control, but has not been shown to improve overall survival[122]. Higher radiation doses up to 60 Gy have been suggested for definitive treatment of unresectable diseases, especially for treating bulky diseases[123].
While most adnexal tumors are resistant to radiation, the role of radiation is not clear due to heterogeneity of tumors. Adjuvant radiotherapy may be considered in patients with microcystic adnexal carcinoma, as well as certain others such as syringocystadenocarcinoma papilliferum and pilomatrix carcinoma[124,125].
SYSTEMIC THERAPY
Immunotherapy has been revolutionary in the management of melanoma, but the role of systemic therapy in NMSC is not clear. Hedgehog pathway inhibitors, and more recently immune checkpoint inhibitors, have been approved for use in metastatic BCC or advanced BCC not amenable to surgery or radiation[126]. For MCC, avelumab, an anti-programmed death-ligand 1 (PD-L1) inhibitor, has been recommended as first-line treatment for metastatic MCC due to results showing median overall survival of 20.3 months with its use in a phase two study[127]. A recent study, in which two-thirds of MCC patients had locoregional disease at presentation, demonstrated that treatment with neoadjuvant nivolumab resulted in a pathological complete response in 47.2%[128].
For advanced unresectable or metastatic SCC, traditional chemotherapy and/or epidermal growth factor receptor inhibitors have been used with modest success, with median overall survival of
Taxanes are the primary treatment in advanced unresectable angiosarcoma, while research on vascular endothelial growth factor inhibitors, checkpoint inhibitors, and eribulin mesylate has not shown significant promise[133]. For adnexal malignancies, chemotherapy may be beneficial in patients with metastatic disease, while anti-estrogenic treatment and human epidermal growth factor receptor 2 inhibitors have been used in some cases with variable outcomes[124].
CONCLUSION
Cutaneous malignancy of the head and neck can spread to the superficial and/or deep lymphatic network, including pre- and post-auricular nodes, parotid nodes, suboccipital nodes, and deep jugular chain nodes, depending on the location and features of the primary tumor. Patient factors such as immunocompromise need to be considered. Clinical evaluation of the parotid and neck should be performed in all patients with head and neck NMSC. Pre-operative imaging is also recommended.
Treatment for lymphatic spread of cutaneous malignancy of the head and neck typically involves surgical resection with adjuvant radiation. Appropriate management of anatomical structures in the head and neck is important to ensure the best surgical outcomes. New systemic therapies, such as cemiplimab, are demonstrating promising results in clinical trials. Management in a multidisciplinary setting is recommended.
DECLARATIONS
Authors’ contributionsMade substantial contributions to conception and design of the study and performed data interpretation and manuscript drafting: Woods RSR, Woods JFC, Fitzgerald CWR, Alameer E, Lopez J, Singh B, Shah JP
Supervised the writing process: Singh B, Shah JP
Approved the final version of the report: Woods RSR, Woods JFC, Fitzgerald CWR, Alameer E, Lopez J, Singh B, Shah JP
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflict of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2022.
REFERENCES
1. Shah JP. Jatin shah’s head and neck surgery and oncology. 5th ed. St. Louis, MO: Elsevier Inc.; 2019.
2. Vauterin TJ, Veness MJ, Morgan GJ, Poulsen MG, O’Brien CJ. Patterns of lymph node spread of cutaneous squamous cell carcinoma of the head and neck. Head Neck 2006;28:785-91.
3. Marks NJ. The anatomy of the lymph nodes of the parotid gland. Clin Otolaryngol Allied Sci 1984;9:271-5.
4. Pisani P, Ramponi A, Pia F. The deep parotid lymph nodes: an anatomical and oncological study. J Laryngol Otol 1996;110:148-50.
5. Stonesifer CJ, Djavid AR, Grimes JM, et al. Immune checkpoint inhibition in non-melanoma skin cancer: a review of current evidence. Front Oncol 2021;11:734354.
6. Franzen A, Buchali A, Lieder A. The rising incidence of parotid metastases: our experience from four decades of parotid gland surgery. Acta Otorhinolaryngol Ital 2017;37:264-9.
7. Swanson MS, Sinha UK. Diagnosis and management of merkel cell carcinoma of the head and neck: current trends and controversies. Cancers (Basel) 2014;6:1256-66.
8. McLean T, Brunner M, Ebrahimi A, et al. Concurrent primary and metastatic cutaneous head and neck squamous cell carcinoma: Analysis of prognostic factors. Head Neck 2013;35:1144-8.
9. Schmults CD, Karia PS, Carter JB, Han J, Qureshi AA. Factors predictive of recurrence and death from cutaneous squamous cell carcinoma: a 10-year, single-institution cohort study. JAMA Dermatol 2013;149:541-7.
10. Khurana VG, Mentis DH, O’brien CJ, Hurst TL, Stevens GN, Packham NA. Parotid and neck metastases from cutaneous squamous cell carcinoma of the head and neck. Am J Surg 1995;170:446-50.
11. Brantsch KD, Meisner C, Schönfisch B, et al. Analysis of risk factors determining prognosis of cutaneous squamous-cell carcinoma: a prospective study. Lancet Oncol 2008;9:713-20.
12. Karia PS, Morgan FC, Ruiz ES, Schmults CD. Clinical and incidental perineural invasion of cutaneous squamous cell carcinoma: a systematic review and pooled analysis of outcomes data. JAMA Dermatol 2017;153:781-8.
13. Rowe DE, Carroll RJ, Day CL. Prognostic factors for local recurrence, metastasis, and survival rates in squamous cell carcinoma of the skin, ear, and lip. J Am Acad Dermatol 1992;26:976-90.
14. Newlands C, Currie R, Memon A, Whitaker S, Woolford T. Non-melanoma skin cancer: United Kingdom National Multidisciplinary Guidelines. J Laryngol Otol 2016;130:S125-32.
15. Haug K, Breuninger H, Metzler G, et al. Prognostic impact of perineural invasion in cutaneous squamous cell carcinoma: results of a prospective study of 1399 tumors. J Invest Dermatol 2020;140:1968-75.
16. Thompson AK, Kelley BF, Prokop LJ, Murad MH, Baum CL. Risk factors for cutaneous squamous cell carcinoma recurrence, metastasis, and disease-specific death: a systematic review and meta-analysis. JAMA Dermatol 2016;152:419-28.
17. Stratigos AJ, Garbe C, Dessinioti C, et al. European interdisciplinary guideline on invasive squamous cell carcinoma of the skin: Part 1. epidemiology, diagnostics and prevention. Eur J Cancer 2020;128:60-82.
18. Harris BN, Bayoumi A, Rao S, Moore MG, Farwell DG, Bewley AF. Factors Associated with Recurrence and Regional Adenopathy for Head and Neck Cutaneous Squamous Cell Carcinoma. Otolaryngol Head Neck Surg 2017;156:863-9.
19. Kearney L, Hogan D, Conlon P, Roche M, O’Neill JP, O’Sullivan JB. High-risk cutaneous malignancies and immunosuppression: Challenges for the reconstructive surgeon in the renal transplant population. J Plast Reconstr Aesthet Surg 2017;70:922-30.
20. Southwell KE, Chaplin JM, Eisenberg RL, McIvor NP, Morton RP. Effect of immunocompromise on metastatic cutaneous squamous cell carcinoma in the parotid and neck. Head Neck 2006;28:244-8.
21. Yilmaz M, Eskiizmir G, Friedman O. Cutaneous squamous cell carcinoma of the head and neck: management of the parotid and neck. Facial Plast Surg Clin North Am 2012;20:473-81.
22. Sahovaler A, Krishnan RJ, Yeh DH, et al. Outcomes of cutaneous squamous cell carcinoma in the head and neck region with regional lymph node metastasis: a systematic review and meta-analysis. JAMA Otolaryngol Head Neck Surg 2019;145:352-60.
23. Porceddu SV, Bressel M, Poulsen MG, et al. Postoperative concurrent chemoradiotherapy versus postoperative radiotherapy in high-risk cutaneous squamous cell carcinoma of the head and neck: the randomized phase iii trog 05.01 trial. J Clin Oncol 2018;36:1275-83.
24. Ch’ng S, Maitra A, Allison RS, et al. Parotid and cervical nodal status predict prognosis for patients with head and neck metastatic cutaneous squamous cell carcinoma. J Surg Oncol 2008;98:101-5.
25. Robsahm TE, Helsing P, Veierød MB. Cutaneous squamous cell carcinoma in Norway 1963-2011: increasing incidence and stable mortality. Cancer Med 2015;4:472-80.
26. Bichakjian CK, Olencki T, Aasi SZ, et al. Merkel cell carcinoma, version 1.2018, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw 2018;16:742-74.
27. Deneve JL, Messina JL, Marzban SS, et al. Merkel cell carcinoma of unknown primary origin. Ann Surg Oncol 2012;19:2360-6.
28. Vandeven N, Lewis CW, Makarov V, et al. Merkel cell carcinoma patients presenting without a primary lesion have elevated markers of immunity, higher tumor mutation burden, and improved survival. Clin Cancer Res 2018;24:963-71.
29. Rizzo JM, Harms PW, Harms KL, Plaska A, Brenner C, Durham AB. Unknown primary Merkel cell carcinoma in the immunosuppressed patient: Case series. JAAD Case Rep 2021;8:19-22.
30. Pan Z, Chen YY, Wu X, et al. Merkel cell carcinoma of lymph node with unknown primary has a significantly lower association with Merkel cell polyomavirus than its cutaneous counterpart. Mod Pathol 2014;27:1182-92.
31. Bajetta E, Celio L, Platania M, et al. Single-institution series of early-stage Merkel cell carcinoma: long-term outcomes in 95 patients managed with surgery alone. Ann Surg Oncol 2009;16:2985-93.
32. Fagan J, Brooks J, Ramsey ML. Basal cell cancer. Treasure Island, FL: StatPearls, 2022.
33. Wysong A, Aasi SZ, Tang JY. Update on metastatic basal cell carcinoma: a summary of published cases from 1981 through 2011. JAMA Dermatol 2013;149:615-6.
34. Morgan FC, Ruiz ES, Karia PS, Besaw RJ, Neel VA, Schmults CD. Factors predictive of recurrence, metastasis, and death from primary basal cell carcinoma 2 cm or larger in diameter. J Am Acad Dermatol 2020;83:832-8.
35. McCusker M, Basset-Seguin N, Dummer R, et al. Metastatic basal cell carcinoma: prognosis dependent on anatomic site and spread of disease. Eur J Cancer 2014;50:774-83.
36. Nguyen-Nielsen M, Wang L, Pedersen L, et al. The incidence of metastatic basal cell carcinoma (mBCC) in Denmark, 1997-2010. Eur J Dermatol 2015;25:463-8.
37. Martinez SR, Barr KL, Canter RJ. Rare tumors through the looking glass: an examination of malignant cutaneous adnexal tumors. Arch Dermatol 2011;147:1058-62.
38. Storino A, Drews RE, Tawa NE Jr. Malignant cutaneous adnexal tumors and role of SLNB. J Am Coll Surg 2021;232:889-98.
39. Barnes M, Hestley A, Murray DR, Carlson GW, Parker D, Delman KA. The risk of lymph node involvement in malignant cutaneous adnexal tumors. Am Surg 2014;80:270-4.
40. Ogata D, Kiyohara Y, Yoshikawa S, Kasami M. Treatment strategy for cutaneous apocrine carcinoma. Int J Clin Oncol 2014;19:712-5.
41. Conic RRZ, Damiani G, Frigerio A, et al. Incidence and outcomes of cutaneous angiosarcoma: A SEER population-based study. J Am Acad Dermatol 2020;83:809-16.
42. Wollina U, Schönlebe J, Bujok V, et al. Dermal pleomorphic sarcoma of the scalp - report of two cases. Open Access Maced J Med Sci 2019;7:2982-4.
44. Sood A, Wykes J, Roshan D, et al. A critical analysis of the prognostic performance of the 8th edition American Joint Committee on Cancer staging for metastatic cutaneous squamous cell carcinoma of the head and neck. Head Neck 2019;41:1591-6.
45. Moody SA, Hirsch BE, Myers EN. Squamous cell carcinoma of the external auditory canal: an evaluation of a staging system. Am J Otol 2000;21:582-8.
46. Ruiz ES, Karia PS, Besaw R, Schmults CD. Performance of the American Joint Committee on Cancer Staging Manual, 8th Edition vs the Brigham and Women’s Hospital Tumor Classification System for Cutaneous Squamous Cell Carcinoma. JAMA Dermatol 2019;155:819-25.
47. Roscher I, Falk RS, Vos L, et al. Validating 4 staging systems for cutaneous squamous cell carcinoma using population-based data: a nested case-control study. JAMA Dermatol 2018;154:428-34.
48. Luk PP, Ebrahimi A, Veness MJ, et al. Prognostic value of the 8th edition American Joint Commission Cancer nodal staging system for patients with head and neck cutaneous squamous cell carcinoma: A multi-institutional study. Head Neck 2021;43:558-67.
49. Ebrahimi A, Luk PP, Low H, et al. The American Joint Committee on Cancer staging for metastatic head and neck cutaneous squamous cell carcinoma: A multi-institutional study of within-stage heterogeneity and impact on prognostic performance. Head Neck 2020;42:3235-42.
50. Amit M, Liu C, Gleber-Netto FO, et al. Inclusion of extranodal extension in the lymph node classification of cutaneous squamous cell carcinoma of the head and neck. Cancer 2021;127:1238-45.
51. Sood A, Wykes J, Roshan D, et al. Number of nodal metastases and prognosis in metastatic cutaneous squamous cell carcinoma of the head and neck. ANZ J Surg 2019;89:863-7.
52. Lubov J, Labbé M, Sioufi K, et al. Prognostic factors of head and neck cutaneous squamous cell carcinoma: a systematic review. J Otolaryngol Head Neck Surg 2021;50:54.
53. Clark JR, Rumcheva P, Veness MJ. Analysis and comparison of the 7th edition American Joint Committee on Cancer (AJCC) nodal staging system for metastatic cutaneous squamous cell carcinoma of the head and neck. Ann Surg Oncol 2012;19:4252-8.
54. Karia PS, Jambusaria-Pahlajani A, Harrington DP, Murphy GF, Qureshi AA, Schmults CD. Evaluation of American Joint Committee on Cancer, International Union Against Cancer, and Brigham and Women’s Hospital tumor staging for cutaneous squamous cell carcinoma. J Clin Oncol 2014;32:327-34.
55. Forest VI, Clark JJ, Veness MJ, Milross C. N1S3: a revised staging system for head and neck cutaneous squamous cell carcinoma with lymph node metastases: results of 2 Australian Cancer Centers. Cancer 2010;116:1298-304.
56. O’Brien CJ, McNeil EB, McMahon JD, Pathak I, Lauer CS, Jackson MA. Significance of clinical stage, extent of surgery, and pathologic findings in metastatic cutaneous squamous carcinoma of the parotid gland. Head Neck 2002;24:417-22.
57. Oddone N, Morgan GJ, Palme CE, et al. Metastatic cutaneous squamous cell carcinoma of the head and neck: the Immunosuppression, Treatment, Extranodal spread, and Margin status (ITEM) prognostic score to predict outcome and the need to improve survival. Cancer 2009;115:1883-91.
58. Moshiri AS, Nghiem P. Milestones in the staging, classification, and biology of Merkel cell carcinoma. J Natl Compr Canc Netw 2014;12:1255-62.
59. Heppt MV, Steeb T, Berking C, Nast A. Comparison of guidelines for the management of patients with high-risk and advanced cutaneous squamous cell carcinoma - a systematic review. J Eur Acad Dermatol Venereol 2019;33 Suppl 8:25-32.
60. Givi B, Andersen PE, Diggs BS, Wax MK, Gross ND. Outcome of patients treated surgically for lymph node metastases from cutaneous squamous cell carcinoma of the head and neck. Head Neck 2011;33:999-1004.
61. O’Brien CJ, McNeil EB, McMahon JD, Pathak I, Lauer CS. Incidence of cervical node involvement in metastatic cutaneous malignancy involving the parotid gland. Head Neck 2001;23:744-8.
62. Thom JJ, Moore EJ, Price DL, Kasperbauer JL, Starkman SJ, Olsen KD. The role of total parotidectomy for metastatic cutaneous squamous cell carcinoma and malignant melanoma. JAMA Otolaryngol Head Neck Surg 2014;140:548-54.
63. Wong WK, Morton RP. Elective management of cervical and parotid lymph nodes in stage N0 cutaneous squamous cell carcinoma of the head and neck: a decision analysis. Eur Arch Otorhinolaryngol 2014;271:3011-9.
64. Peiffer N, Kutz JW Jr, Myers LL, et al. Patterns of regional metastasis in advanced stage cutaneous squamous cell carcinoma of the auricle. Otolaryngol Head Neck Surg 2011;144:36-42.
65. Yoon M, Chougule P, Dufresne R, Wanebo HJ. Localized carcinoma of the external ear is an unrecognized aggressive disease with a high propensity for local regional recurrence. Am J Surg 1992;164:574-7.
66. Mazzoni A, Danesi G, Zanoletti E. Primary squamous cell carcinoma of the external auditory canal: surgical treatment and long-term outcomes. Acta Otorhinolaryngol Ital 2014;34:129-37.
67. Kadakia S, Saman M, Gordin E, Marra D, Ducic Y. The role of parotidectomy in the treatment of auricular squamous cell carcinoma. Otolaryngol Head Neck Surg 2015;152:1048-52.
68. Kadakia S, Ducic Y, Marra D, Saman M. The role of elective superficial parotidectomy in the treatment of temporal region squamous cell carcinoma. Oral Maxillofac Surg 2016;20:143-7.
69. Skulsky SL, O’Sullivan B, McArdle O, et al. Review of high-risk features of cutaneous squamous cell carcinoma and discrepancies between the American Joint Committee on Cancer and NCCN Clinical Practice Guidelines in Oncology. Head Neck 2017;39:578-94.
70. Amit M, Liu C, Mansour J, et al. Elective neck dissection versus observation in patients with head and neck cutaneous squamous cell carcinoma. Cancer 2021;127:4413-20.
71. Tremblay-Abel V, Poulin MA, Blouin MM, Parent F, Perron É. Sentinel lymph node biopsy in high-risk cutaneous squamous cell carcinoma: analysis of a large size retrospective series. Dermatol Surg 2021;47:908-13.
72. Keohane SG, Botting J, Budny PG, et al. British Association of Dermatologists guidelines for the management of people with cutaneous squamous cell carcinoma 2020. Br J Dermatol 2021;184:401-14.
73. Sapijaszko M, Zloty D, Bourcier M, Poulin Y, Janiszewski P, Ashkenas J. Canadian Non-melanoma Skin Cancer Guidelines Committee. Non-melanoma skin cancer in Canada chapter 5: management of squamous cell carcinoma. J Cutan Med Surg 2015;19:249-59.
74. Harwood M, Wu H, Tanabe K, Bercovitch L. Metastatic basal cell carcinoma diagnosed by sentinel lymph node biopsy. J Am Acad Dermatol 2005;53:475-8.
75. Picon AI, Coit DG, Shaha AR, et al. Sentinel lymph node biopsy for cutaneous head and neck melanoma: mapping the parotid gland. Ann Surg Oncol 2016;23:9001-9.
77. Hirshoren N, Ruskin O, McDowell LJ, Magarey M, Kleid S, Dixon BJ. Management of Parotid Metastatic Cutaneous Squamous Cell Carcinoma: Regional Recurrence Rates and Survival. Otolaryngol Head Neck Surg 2018;159:293-9.
78. Audet N, Palme CE, Gullane PJ, et al. Cutaneous metastatic squamous cell carcinoma to the parotid gland: analysis and outcome. Head Neck 2004;26:727-32.
79. Ebrahimi A, Moncrieff MD, Clark JR, et al. Predicting the pattern of regional metastases from cutaneous squamous cell carcinoma of the head and neck based on location of the primary. Head Neck 2010;32:1288-94.
80. Olsen KD, Quer M, de Bree R, Vander Poorten V, Rinaldo A, Ferlito A. Deep lobe parotidectomy-why, when, and how? Eur Arch Otorhinolaryngol 2017;274:4073-8.
81. Cracchiolo JR, Shaha AR. Parotidectomy for Parotid Cancer. Otolaryngol Clin North Am 2016;49:415-24.
82. Veness MJ, Porceddu S, Palme CE, Morgan GJ. Cutaneous head and neck squamous cell carcinoma metastatic to parotid and cervical lymph nodes. Head Neck 2007;29:621-31.
83. Goh RY, Bova R, Fogarty GB. Cutaneous squamous cell carcinoma metastatic to parotid - analysis of prognostic factors and treatment outcome. World J Surg Oncol 2012;10:117.
84. Shao A, Wong DK, McIvor NP, et al. Parotid metastatic disease from cutaneous squamous cell carcinoma: prognostic role of facial nerve sacrifice, lateral temporal bone resection, immune status and P-stage. Head Neck 2014;36:545-50.
85. Woods RSR, Naude A, O’Sullivan JB, et al. Management of temporal bone malignancy in treland. J Neurol Surg B Skull Base 2020;81:680-5.
86. Esclamado RM, Carroll WR. Extracapsular spread and the perineural extension of squamous cell cancer in the cervical plexus. Arch Otolaryngol Head Neck Surg 1992;118:1157-8.
87. Yesensky J, Solis RN, Bewley A. Facial nerve sacrifice during parotidectomy for metastatic cutaneous squamous cell carcinoma. OTO Open 2021;5:2473974X21996627.
88. Solares CA, Lee K, Parmar P, O’Rourke P, Panizza B. Epidemiology of clinical perineural invasion in cutaneous squamous cell carcinoma of the head and neck. Otolaryngol Head Neck Surg 2012;146:746-51.
89. Panizza B, Solares CA, Redmond M, Parmar P, O’Rourke P. Surgical resection for clinical perineural invasion from cutaneous squamous cell carcinoma of the head and neck. Head Neck 2012;34:1622-7.
90. Warren TA, Panizza B, Porceddu SV, et al. Outcomes after surgery and postoperative radiotherapy for perineural spread of head and neck cutaneous squamous cell carcinoma. Head Neck 2016;38:824-31.
91. Solares CA, Mason E, Panizza BJ. Surgical management of perineural spread of head and neck cancers. J Neurol Surg B Skull Base 2016;77:140-9.
92. Kwok HC, Morton RP, Chaplin JM, McIvor NP, Sillars HA. Quality of life after parotid and temporal bone surgery for cancer. Laryngoscope 2002;112:820-33.
93. Swendseid BP, Philips RHW, Rao NK, et al. The underappreciated role of auriculotemporal nerve involvement in local failure following parotidectomy for cancer. Head Neck 2020;42:3253-62.
94. Iwanaga J, Fisahn C, Watanabe K, et al. Parotid Branches of the Auriculotemporal Nerve: An Anatomical Study With Implications for Frey Syndrome. J Craniofac Surg 2017;28:262-4.
95. Tansatit T, Apinuntrum P, Phetudom T. Evidence suggesting that the buccal and zygomatic branches of the facial nerve May contain parasympathetic secretomotor fibers to the parotid gland by means of communications from the auriculotemporal nerve. Aesthetic Plast Surg 2015;39:1010-7.
96. Lebbe C, Becker JC, Grob JJ, et al. Diagnosis and treatment of Merkel Cell Carcinoma. European consensus-based interdisciplinary guideline. Eur J Cancer 2015;51:2396-403.
97. Amin MB, Edge SB, Gress DM, et al. American Joint Committee on Cancer, American Cancer Society. AJCC cancer staging manual. 8th ed.Chicago, IL, USA: American Joint Committee on Cancer, Springer, 2017.
98. Lee JS, Durham AB, Bichakjian CK, et al. Completion lymph node dissection or radiation therapy for sentinel node metastasis in merkel cell carcinoma. Ann Surg Oncol 2019;26:386-94.
99. Al-Hakami H, Awad BI, Al-Garni M, Al-Maghrabi HA, Al-Shareef N. Apocrine carcinoma of the scalp with neck lymph node metastasis: A case report and review of the literature. J Family Med Prim Care 2019;8:3758-62.
100. Casso C, Kwhaja S, Davies S, Al-Ani Z, Saeed SR, Homer JJ. Effect of temporal bone resection on temporomandibular joint function: a quality of life study. Otolaryngol Head Neck Surg 2010;142:85-9.
101. Haymerle G, Enzenhofer E, Lechner W, et al. The effect of adjuvant radiotherapy on radial forearm free flap volume after soft palate reconstruction in 13 patients. Clin Otolaryngol 2018;43:742-5.
102. Rowe D, Emmett J. Reconstruction of the Base of Skull Defect-Lessons Learned over 25 Combined Years. J Neurol Surg B Skull Base 2016;77:161-8.
103. Rosenthal EL, King T, McGrew BM, Carroll W, Magnuson JS, Wax MK. Evolution of a paradigm for free tissue transfer reconstruction of lateral temporal bone defects. Head Neck 2008;30:589-94.
104. Urban MJ, Eggerstedt M, Varelas E, et al. Hypoglossal and Masseteric Nerve Transfer for Facial Reanimation: A Systematic Review and Meta-Analysis. Facial Plast Surg Aesthet Med 2022;24:10-7.
105. Herman MP, Amdur RJ, Werning JW, Dziegielewski P, Morris CG, Mendenhall WM. Elective neck management for squamous cell carcinoma metastatic to the parotid area lymph nodes. Eur Arch Otorhinolaryngol 2016;273:3875-9.
106. Nottage MK, Lin C, Hughes BG, et al. Prospective study of definitive chemoradiation in locally or regionally advanced squamous cell carcinoma of the skin. Head Neck 2017;39:679-83.
107. Wang JT, Palme CE, Morgan GJ, Gebski V, Wang AY, Veness MJ. Predictors of outcome in patients with metastatic cutaneous head and neck squamous cell carcinoma involving cervical lymph nodes: Improved survival with the addition of adjuvant radiotherapy. Head Neck 2012;34:1524-8.
108. Veness MJ, Morgan GJ, Palme CE, Gebski V. Surgery and adjuvant radiotherapy in patients with cutaneous head and neck squamous cell carcinoma metastatic to lymph nodes: combined treatment should be considered best practice. Laryngoscope 2005;115:870-5.
109. Porceddu SV, Daniels C, Yom SS, et al. Head and Neck Cancer International Group (HNCIG) Consensus Guidelines for the Delivery of Postoperative Radiation Therapy in Complex Cutaneous Squamous Cell Carcinoma of the Head and Neck (cSCCHN). Int J Radiat Oncol Biol Phys 2020;107:641-51.
110. Tanvetyanon T, Padhya T, McCaffrey J, et al. Postoperative concurrent chemotherapy and radiotherapy for high-risk cutaneous squamous cell carcinoma of the head and neck. Head Neck 2015;37:840-5.
111. Goyal U, Prabhakar NK, Davuluri R, Morrison CM, Yi SK. Role of Concurrent Systemic Therapy with Adjuvant Radiation Therapy for Locally Advanced Cutaneous Head and Neck Squamous Cell Carcinoma. Cureus 2017;9:e1784.
112. Lavaud J, Blom A, Longvert C, Fort M, Funck-Brentano E, Saiag P. Pembrolizumab and concurrent hypo-fractionated radiotherapy for advanced non-resectable cutaneous squamous cell carcinoma. Eur J Dermatol 2019;29:636-40.
113. Joseph K, Walker J, Raziee H, Faruqi S, Smylie M. PD-1 Blockade With Concurrent Radiotherapy for Locally Advanced Inoperable Cutaneous Squamous Cell Carcinoma. J Cutan Med Surg 2022;26:243-8.
114. Vaidya P, Mehta A, Ragab O, Lin S, In GK. Concurrent radiation therapy with programmed cell death protein 1 inhibition leads to a complete response in advanced cutaneous squamous cell carcinoma. JAAD Case Rep 2019;5:763-6.
115. Bishop AJ, Garden AS, Gunn GB, et al. Merkel cell carcinoma of the head and neck: Favorable outcomes with radiotherapy. Head Neck 2016;38 Suppl 1:E452-8.
116. Strom T, Naghavi AO, Messina JL, et al. Improved local and regional control with radiotherapy for Merkel cell carcinoma of the head and neck. Head Neck 2017;39:48-55.
117. Gunaratne DA, Howle JR, Veness MJ. Sentinel lymph node biopsy in Merkel cell carcinoma: a 15-year institutional experience and statistical analysis of 721 reported cases. Br J Dermatol 2016;174:273-81.
118. Lok B, Khan S, Mutter R, et al. Selective radiotherapy for the treatment of head and neck Merkel cell carcinoma. Cancer 2012;118:3937-44.
119. Tseng YD, Apisarnthanarax S, Liao JJ, Bhatia S, Nghiem PT, Parvathaneni U. Factors influencing radiation treatment recommendations in early-stage Merkel cell carcinoma: a survey of US-based radiation oncologists. Expert Rev Anticancer Ther 2017;17:281-7.
120. Jouary T, Leyral C, Dreno B, et al. Adjuvant prophylactic regional radiotherapy versus observation in stage I Merkel cell carcinoma: a multicentric prospective randomized study. Ann Oncol 2012;23:1074-80.
121. Cook MM, Schaub SK, Goff PH, et al. Postoperative, Single-Fraction Radiation Therapy in Merkel Cell Carcinoma of the Head and Neck. Adv Radiat Oncol 2020;5:1248-54.
122. Bhatia S, Storer BE, Iyer JG, et al. Adjuvant radiation therapy and chemotherapy in merkel cell carcinoma: survival analyses of 6908 cases from the national cancer data base. J Natl Cancer Inst 2016;108:djw042.
123. Rush Z, Fields RC, Lee N, Brownell I. Radiation therapy in the management of Merkel cell carcinoma: current perspectives. Expert Rev Dermatol 2011;6:395-404.
124. Płachta I, Kleibert M, Czarnecka AM, Spałek M, Szumera-Ciećkiewicz A, Rutkowski P. Current Diagnosis and Treatment Options for Cutaneous Adnexal Neoplasms with Apocrine and Eccrine Differentiation. Int J Mol Sci 2021;22:5077.
125. Płachta I, Kleibert M, Czarnecka AM, Spałek M, Szumera-Ciećkiewicz A, Rutkowski P. Current Diagnosis and Treatment Options for Cutaneous Adnexal Neoplasms with Follicular Differentiation. Int J Mol Sci 2021;22:4759.
126. Dessinioti C, Plaka M, Soura E, et al. A Practical Guide for the Follow-Up of Patients with Advanced Basal Cell Carcinoma During Treatment with Hedgehog Pathway Inhibitors. Oncologist 2019;24:e755-64.
127. D’Angelo SP, Lebbé C, Mortier L, et al. First-line avelumab in a cohort of 116 patients with metastatic Merkel cell carcinoma (JAVELIN Merkel 200): primary and biomarker analyses of a phase II study. J Immunother Cancer 2021;9:e002646.
128. Topalian SL, Bhatia S, Amin A, et al. Neoadjuvant Nivolumab for Patients With Resectable Merkel Cell Carcinoma in the CheckMate 358 Trial. J Clin Oncol 2020;38:2476-87.
129. Cowey CL, Robert NJ, Espirito JL, et al. Clinical outcomes among unresectable, locally advanced, and metastatic cutaneous squamous cell carcinoma patients treated with systemic therapy. Cancer Med 2020;9:7381-7.
130. Migden MR, Rischin D, Schmults CD, et al. PD-1 Blockade with Cemiplimab in Advanced Cutaneous Squamous-Cell Carcinoma. N Engl J Med 2018;379:341-51.
131. Hughes BGM, Munoz-Couselo E, Mortier L, et al. Pembrolizumab for locally advanced and recurrent/metastatic cutaneous squamous cell carcinoma (KEYNOTE-629 study): an open-label, nonrandomized, multicenter, phase II trial. Ann Oncol 2021;32:1276-85.
132. Maubec E, Boubaya M, Petrow P, et al. Phase II Study of Pembrolizumab As First-Line, Single-Drug Therapy for Patients With Unresectable Cutaneous Squamous Cell Carcinomas. J Clin Oncol 2020;38:3051-61.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Woods RSR, Woods JFC, Fitzgerald CWR, Alameer E, Lopez J, Singh B, Shah JP. Lymph node metastasis from non-melanoma skin cancer. J Cancer Metastasis Treat 2022;8:22. http://dx.doi.org/10.20517/2394-4722.2022.28
AMA Style
Woods RSR, Woods JFC, Fitzgerald CWR, Alameer E, Lopez J, Singh B, Shah JP. Lymph node metastasis from non-melanoma skin cancer. Journal of Cancer Metastasis and Treatment. 2022; 8(5): 22. http://dx.doi.org/10.20517/2394-4722.2022.28
Chicago/Turabian Style
Woods, Robbie S. R., Jack F. C. Woods, Conall W. R. Fitzgerald, Ehab Alameer, Joseph Lopez, Bhuvanesh Singh, Jatin P. Shah. 2022. "Lymph node metastasis from non-melanoma skin cancer" Journal of Cancer Metastasis and Treatment. 8, no.5: 22. http://dx.doi.org/10.20517/2394-4722.2022.28
ACS Style
Woods, RSR.; Woods JFC.; Fitzgerald CWR.; Alameer E.; Lopez J.; Singh B.; Shah JP. Lymph node metastasis from non-melanoma skin cancer. J. Cancer. Metastasis. Treat. 2022, 8, 22. http://dx.doi.org/10.20517/2394-4722.2022.28
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 24 clicks
Cite This Article 24 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.