Minimally invasive transthoracic resection of a segment eight liver tumor
Abstract
Despite advances in technology and technique of minimally invasive liver surgery, resection of lesions in the posterosuperior segments such as segment 8 (S8) remains challenging. Compared to open surgery, there are specific differences that make minimally invasive access to S8 challenging. These include the caudal view along the axis of the hepatoduodenal ligament, increased distance between trocars and the operative field, and the liver fulcrum created by the anterolateral segments limiting the view. However, several advancements have helped to overcome these challenges, such as the use of intercostal trocars (combined lateral-abdominal approach) and a flexible tip camera. Consequently, a total thoracoscopic (transthoracic) approach was developed to resect subdiaphragmatic tumors, which may particularly benefit patients with a hostile abdomen. This article summarizes the anatomic, technical, and technological considerations for safe resection of lesions in S8.
Keywords
INTRODUCTION
The safety of minimally invasive liver surgery (MILS) has increased over the last two decades because of advanced accuracy in patient selection and improvement in surgical techniques and postoperative management[1,2]. MILS is associated with reduced transfusion rate and hospital stay with similar operation time, surgical margins and long-term results when compared to open surgery[3-5]. In particular, MILS is frequently considered as the standard approach for selected procedures, such as left lateral sectionectomy. Nevertheless, MILS may still represent clinical challenges, particularly when approaching posterosuperior (PS) segments (S1, S4a, S7, S8)[6-9]. While at the beginning of the MILS experience, these segments were considered to be inaccessible through a MILS approach, our group and others have put forward specific techniques and technology that facilitate access to these segments.
Several classifications have been published, attempting to label MILS based on the technical difficulty of the procedure, instead of just considering the number of segments resected or the anatomical fashion of the resection, as in the Brisbane classification[7-10]. The classification proposed by Kawaguchi et al.[8] includes segmentectomies of PS segments among grade III, high level procedures, and the updated scoring system for difficulty index by Wakabayashi et al.[7] associates a high score with tumors located in PS segments.
When performing MILS, the axis of the operative view (laparoscopic caudal view) is different than in the open approach. The axis of the MILS surgical view is caudal to cranial, while in open surgery, the view is anterior to posterior (ventral approach). The laparoscopic view may facilitate the visualization of the portal structure and the caudate lobe, due to the rib cage overlying most of the liver. Nevertheless, it is difficult for the MILS viewing axis to overcome the fulcrum of the liver and allow for good visualization of the PS segments, such as S8[11-13]. Several groups, including ours, have described approaches that facilitate viewing the PS segments. These approaches have been shown to be safe and feasible when performed by experienced minimally invasive hepato-biliary surgeons[6,14-24]. Among the PS segments, S8 is particularly challenging due to its complex anatomy and large size[25-32]. Here, we present in detail a novel approach that aims at facilitating access to S8, called the transthoracic approach.
ANATOMY OF SEGMENT 8
The right hemiliver is divided into two sections by the right portal fissure. The right hepatic vein (RHV) runs along the right portal fissure dividing the right liver into the right anterior (S5-S8) and right posterior (S6-S7) sections. Hence, the lateral border of S8 is the RHV. The medial border of S8 is the middle hepatic vein (MHV). The inferior border is cephalad to the portal bifurcation[33]. Further, it is key to understand the anatomy of the portal pedicle to S8 and its constant variants. The portal pedicle for S8 (P8) is located deep in the liver parenchyma (S8 is the largest liver segment), and branches into a ventral (P8v) and dorsal (P8d) pedicle in 75% of patients, feeding the ventral and dorsal subsegments, respectively[34-36]. P8d is the first branch ascending from the right anterior portal pedicle. In most patients, P8d gives rise to dorsally directed branches, posterior to the RHV, reaching the dorsocranial area of the right hepatic hemiliver, posterior to the RHV[36]. Hence, it is important to understand that S8 can reach laterally beyond the RHV. An anterior fissure vein (AFV) runs between the ventral and dorsal subsegments and may drain into either the RHV or the MHV. A dominant AFV is found in up to 45% of patients and may be a helpful landmark when performing an anatomical subsegmentectomy[37,38].
CLASSIFICATION OF LAPAROSCOPIC LIVER RESECTIONS
Several authors have developed classification systems to assess the difficulty of MILS based on the concept that the traditional distinction of minor vs. major hepatectomy does not reflect technical challenges and postoperative outcomes[7-9].
Wakabayashi et al. reported four levels of difficulty (low, intermediate, advanced, and expert), assigned to a 0-12 point scoring system[7]. In this classification system, six variables are being scored: tumor location
Kawaguchi et al. described three difficulty levels according to three intraoperative variables: operative time, estimated blood loss, and conversion rate[8]. Grade III refers to a complicated procedure, which includes segmentectomy of PS segments and right posterior sectionectomy. Grade III procedures were associated with longer operative time, higher conversion rate, higher estimated blood loss and higher morbidity rate. Following validation with an external cohort of patients, the rates of liver failure, bile leakage, fluid collection, and pulmonary complications were associated with an increased difficulty grade[9]. Both classifications acknowledge procedures involving PS segments as challenging, especially when anatomic segmentectomies are performed.
THE “CAUDAL VIEW” CONCEPT
A substantial difference between open surgery and MILS is the surgical view. The open ventral approach limits the visualization of the adrenal glands, the inferior vena cava (IVC), and the dorsal side of the porta. The caudal laparoscopic view allows for a direct view of the porta directly in front of the camera. It provides a more direct view of the IVC, and the dorsal side of the hilar plate compared to an open view[11,12].
THE CHALLENGE OF SEGMENT 8
Isolated anatomic S8 resection is challenging since S8 is the biggest liver segment. Like all segments of the liver, anatomical landmarks are not directly visible on its surface. As a result, intraoperative ultrasound (IOUS) utilization is critical. When resecting tumors located deep in S8, the caudal view limits a direct visualization of the resection area because the anterior segments obstruct the view. This is also known as the “fulcrum effect”[14]. Furthermore, the increased distance between the laparoscope, the operative trocars and the resection area, together with the straight structure of most laparoscopic instruments, lead to poor surgical visualization of the surgical field and the difficulty in developing a transection plane. This impacts the control of bleeding and the identification of surgical margins[20,38]. While some technological innovations, such as a flexible tip camera, are helping to overcome the fulcrum, S8 remains a challenging segment to access.
A recent international multicenter propensity-score matched study showed a greater difficulty of laparoscopic atypical resection of S7 compared to S8, and greater difficulty of segmentectomy 8 compared to segmentectomy 7[39].
SURGICAL TECHNIQUE
S8 resection can be differentiated into anatomical and non-anatomical resection. First, the drainage of the MHV and RHV into the IVC is identified using intraoperative ultrasound[37]. The parenchymal transection may either start from the hepatic venous confluence inferiorly, or upwards from the hilum. Most approaches start the parenchymal transection at the Cantlie line, to the right of the MHV, to allow for isolation of P8 deep within the liver parenchyma (transfissural approach). Alternatively, P8 may be identified following the Glissonean pedicle into the liver from the hilum (Glissonean or Takasaki approach). Another approach uses IOUS to identify the right anterior pedicle, followed by transection of a small bridge of parenchyma on the ventral liver surface to identify P8 (transparenchymal approach). Early P8 clamping is useful for allowing demarcation of the right-sided resection margin, which is to the left of the RHV[33,37,38]. Alternatively, a dye or indocyanine green can be injected directly into P8 to stain the segment.
For the transfissural approach, the transection extends along the right side of the MHV, exposing it from the IVC confluence to the periphery. Venous branches draining into the MHV (including the AFV) are divided. In case of a S8 dorsal (S8d) anatomic resection, the dissection runs along the AFV. The resection continues between S8 and S5, where a dominant MHV drainage vein is usually found. P8 lies deep along this plane and can be divided at this point. In case of anatomic subsegmentomies, only P8v or P8d would be ligated. To maintain the correct transection plane on the right side, it is necessary to proceed again from the cranial side, exposing the RHV at its confluence and continuing to the periphery. S8 resection is completed by separating the remaining parenchyma from the IVC[33,37,38].
The concepts of preventing a positive dorsal margin are similar to a non-thoracic approach. Having a low entry angle of the approach to the lesion and a steep exit angle of the transection plane minimizes the risk.
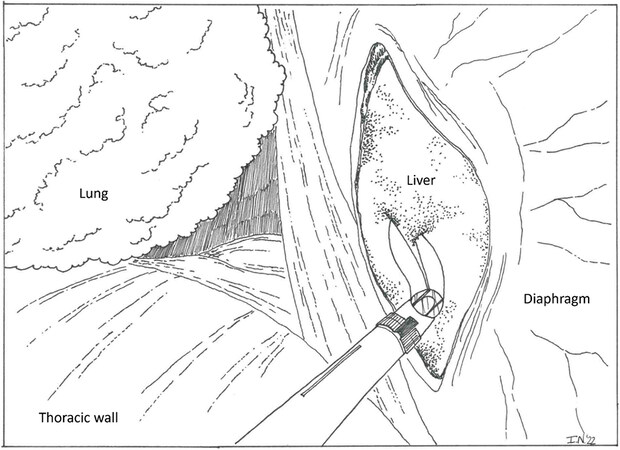
The surgical view of the total transthoracic approach is depicted in Figure 1.
THE TRANSDIAPHRAGMATIC APPROACH
Given the special difficulties associated with MILS S8 resection, several techniques have been described to simplify this procedure.
The use of intercostal trocars was first described by Ishizawa et al. to facilitate the exposure of the roots of MHV and RHV during segmentectomies 7 and 8[40]. First, the patient is placed in the modified French position: with the legs in stirrups, the upper body in the left lateral decubitus position and the right arm suspended. In addition to three trocars in the abdomen, two balloon-tipped trocars (10 mm and 5 mm) are placed through the same intercostal space. At the completion of the case, all gas (room air, more important than the fast-absorbing CO2) that may have accessed the chest is aspirated. Hence, chest tubes are not required. Using this approach, neither lung injury nor postoperative pneumothorax was recorded.
The same authors later reported a series of 44 patients undergoing parenchyma-sparing laparoscopic resection of S7 and S8, 25 of which were approached in this lateral-abdominal fashion[15]. In their updated technique, four to five abdominal trocars were placed in the right upper abdomen, with three under the subcostal arch. After fully mobilizing the right liver, the parenchymal transection of the caudal and superficial liver parenchyma is accomplished through abdominal trocars. Then, the surgeon moves laterally to the right of the patient. Due to the placement of intercostal trocars, instrument triangulation is optimized. The benefit of this approach is a close-up visualization of the transection plane. In this series, the combined lateral-abdominal approach (CLA) was associated with the reduced rate of blood transfusion and conversion.
Lee et al. reported on the non-anatomic resection of small lesions in S7 and S8[41]. In this series, the authors placed four abdominal trocars and two intercostal trocars at the 7th and 9th intercostal space, emphasizing how trocars should be placed on top of the superior margin of the rib to avoid neuro-vascular injury. Similar to the prior reports, there were no lung injuries, and the procedure was performed without single lung ventilation.
Inoue et al. showed a lower conversion rate when using intercostal trocars for resections of S6, S7 and S8[42]. Two 5 mm ports with balloons were placed between the 7th and the 10th intercostal spaces. Before insertion, the lower edge of the lung was identified on ultrasound. Trocars were placed after lung collapse. Inserting the camera through the intercostal trocars allowed the surgeon to form a triangle with the laparoscope in the center, maintaining the co-axial position from the right lateral side of the liver. When comparing the total abdominal approach to CLA for the resection of tumors in S7 and S8, Hirokawa et al. demonstrated prolonged surgical time, increased bleeding, and a higher conversion rate with the traditional approach[43].
THE TRANSTHORACIC APPROACH
Following the development of the transdiaphragmatic technique, where trocars are placed through the diaphragm into the abdominal cavity, a total transthoracic thoracoscopic approach was developed[44-47]. For this technique, ports are placed into the chest and the liver is approached after opening the diaphragm [Figure 1].
Indication
A tumor located in the very posterior superior liver is best suited for a transthoracic liver resection. The target lesion is ideally located just below the diaphragm, which is easiest evaluated in the coronal plane on axial imaging[48-55]. While Teramoto et al.[49,50] and Qin et al.[56] suggested a 3 cm tumor size cut-off for selection of patients, Zhu et al.[55] believed that this approach should be considered in patients with 3-5 cm superficial subphrenic tumors, distant from the RHV or IVC. Ishizawa et al. have demonstrated that large lesions in close contact with the IVC or the hepatic veins are amendable to this approach[40]. Nonetheless, the size of the tumor not only affects the extent and difficulty of the liver resection itself, but it also needs to be considered for the extraction of the specimen through the thoracic wall[51].
This approach is ideally suited for patients who underwent prior laparotomies, liver resections, or
Review of literature
Teramoto et al. first described the utilization of a total thoracoscopic transthoracic approach[49,50]. In two consecutive reports, the authors recommended this strategy to resect or ablate hepatocellular carcinoma (HCC) located in subdiaphragmatic S8. They placed five trocars in the intercostal spaces at different levels. The diaphragm was opened with ultrasonic scissors or by electronic cautery. Using thoracoscopic ultrasound to identify the tumor, the hepatectomy was performed with an ultrasonic tissue dissector and a microwave tissue coagulator.
Cloyd et al. reported two cases of video-assisted thoracoscopic transdiaphragmatic resection of HCC located in S7 and S8, respectively[51]. The first case involved an obese patient with a 2 cm mass in S7 that had already undergone laparoscopic radiofrequency. The second included a patient with a recurrent 2 cm HCC nodule in S8 who underwent an open right posterior sectionectomy 18 months prior. The authors described their technique, emphasizing the importance of a left lateral decubitus flexed position, the necessity for
Aikawa et al. described a case of a recurrent 1.5 cm colorectal liver metastasis at the dome of S8, with a history of laparoscopic sigmoidectomy and posterior segmentectomy of the liver[52]. Based on both the location of the tumor and the risk of significant adhesions, a transthoracic approach was selected. In this case, three trocars were placed in the right thoracic space.
Yamashita et al. demonstrated a successful procedure for a severely obese patient with a recurrent S8 colorectal liver metastasis, who previously underwent rectosigmoid resection, partial resection of S5-8 and S2-3, radiofrequency ablation for S7, and left hepatectomy with common bile duct resection and choledochojejunostomy[54]. The patient underwent preoperative chemotherapy with four cycles of
Hallet et al. focused on the role of augmented reality[53]. The role of augmented reality in managing thoracic port placement, choice of phrenotomy site and identification of the parenchymal transection line was detailed. The authors emphasized how the phrenotomy should be limited in length and performed towards the periphery to avoid phrenic injury, preventing incision of the diaphragm radially.
Zhu et al. reported six cases, two involving tumors in S8 and four in S7[55]. Each procedure involved superficial HCC nodules in the context of chronic hepatitis B. Only two patients had a history of previous abdominal surgery. The technique described is different from the previous reports: an initial transabdominal approach was used to encircle the hepatoduodenal ligament (except for the left hepatic artery). The tape used for this maneuver was exteriorized through a subxiphoid trocar to allow for the Pringle maneuver. Then, patients were positioned in the traditional left lateral position and three thoracic trocars were placed in the 6th intercostal space on the right posterior axillary line, and in the 3rd and 8th intercostal spaces on the right middle axillary line, respectively.
Qin et al. described the case of a cirrhotic patient with a 1.3 cm HCC in S8[56]. Three trocars were placed into the right thoracic space. The technique was similar to previous reports, but the authors performed intraoperative RFA around the tumor before starting the resection. This approach reduced the risk of blood loss and helped to achieve tumor-free surgical margins.
Table 1 summarizes the reports detailed above, describing minimally invasive total transthoracic approach for liver resection of S8.
A summary of papers describing minimally invasive total transthoracic approach for liver resection of segment 8
| Author | Teramoto et al.[50] | Cloyd and Visser[51] | Aikawa et al.[52] | Hallet et al.[53] | Yamashita et al.[54] | Zhu et al.[55] | Qin et al.[56] |
| Year | 2005 | 2011 | 2014 | 2015 | 2016 | 2019 | 2019 |
| No. of patients | 5 | 2 | 1 | 1 | 1 | 6 | 1 |
| Indication | HCC | HCC | CLM | HCC | CLM | HCC | HCC |
| Tumor size, cm, median | NA* | 2.1 (2-2.3) | 1.5 | 4 | NA | 3.7 (1.5-4) | 1.3 |
| Cirrhosis | NA* | 1/2 | No | No | No | Hepatitis B | Yes |
| Number of trocars | 5 | 3 | 3 | 4 | 3-5 | 6 (3 abdominal) | 3 |
| Vascular inflow control | No | No | No | No | No | Yes | No |
| “Hemostatic” RFA | No | 1/2 | No | No | No | No | Yes |
| Anatomical resection | No | No | No | No | No | No | No |
| Transection device | UTD | RFA/BTT | BTT | UTD | BTT/UTD | UTD | NA |
| Diaphragm suture | NA | Running/interrupted | Running | NA | Running | Running | NA |
| Chest tube placement | No | Yes | No | Yes | Yes | Yes | Yes |
| Blood loss, mL, median | NA* | NA | 10 | 300 | 100 | 60 (30-120) | 50 |
| Operative time, minutes, median | NA* | NA | 310 | 270 | 247 | 140 | 210 |
| Margin status | NA | Negative | NA | NA | Negative | NA | NA |
| Complications | NA* | No | No | No | No | 1/6 | No |
Limitations
The main limitations to the transthoracic approach are the lack of inflow control and the impossibility of retrieving voluminous specimens from the intercostal space, making it unfavorable to perform anatomical resections.
A recent meta-analysis by Pathak et al. underlined how minimally invasive transthoracic liver surgery has not yet become a widely popular approach, even if previous reports describe it as safe and feasible[57]. The authors point out that the aforementioned papers do not provide enough homogeneous and technical detail. None of the reported studies mentioned the learning curve for this procedure, the surgeons’ level of experience, nor adhered to the IDEAL framework. The IDEAL framework describes the stages through which every surgical therapy innovation should normally pass, describing the characteristics of each of the five stages: Idea, Development, Exploration, Assessment, and Long-term follow-up. According to the IDEAL framework, this technique would be defined as stage 2a (development stage).
CONCLUSION
Transdiaphragmatic and transthoracic approaches are important tools in the armamentarium of the advanced minimally invasive liver surgeon. The transdiaphragmatic approach helps to optimize triangulation and visualization of lesions in S8. The total thoracoscopic transthoracic approach is a safe and feasible procedure in patients with small subdiaphragmatic tumors. It is particularly useful for patients that underwent multiple previous abdominal surgeries and for cirrhotic patients waiting for liver transplantation. The main disadvantage of the transthoracic approach is the lack of inflow control and the impossibility of retrieving voluminous specimens from the intercostal space.
DECLARATIONS
Authors’ contributionsMade substantial contributions to conception, design, and editing of the manuscript: Panettieri E, Vega EA, Conrad C
Availability of data and materialsNot applicable.
Financial support and sponsorshipNone.
Conflicts of interestAll authors declared that there are no conflicts of interest.
Ethical approval and consent to participateNot applicable.
Consent for publicationNot applicable.
Copyright© The Author(s) 2023.
REFERENCES
1. Kaibori M, Yoshii K, Hasegawa K, et al. Treatment optimization for hepatocellular carcinoma in elderly patients in a Japanese nationwide cohort. Ann Surg 2019;270:121-30.
2. Bryant R, Laurent A, Tayar C, Cherqui D. Laparoscopic liver resection-understanding its role in current practice: the Henri Mondor Hospital experience. Ann Surg 2009;250:103-11.
3. Takahara T, Wakabayashi G, Beppu T, et al. Long-term and perioperative outcomes of laparoscopic versus open liver resection for hepatocellular carcinoma with propensity score matching: a multi-institutional Japanese study. J Hepatobiliary Pancreat Sci 2015;22:721-7.
4. Sposito C, Battiston C, Facciorusso A, et al. Propensity score analysis of outcomes following laparoscopic or open liver resection for hepatocellular carcinoma. Br J Surg 2016;103:871-80.
5. Fretland ÅA, Dagenborg VJ, Bjørnelv GMW, et al. Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg 2018;267:199-207.
6. Abu Hilal M, Aldrighetti L, Dagher I, et al. The southampton consensus guidelines for laparoscopic liver surgery: from indication to implementation. Ann Surg 2018;268:11-8.
7. Wakabayashi G. What has changed after the Morioka consensus conference 2014 on laparoscopic liver resection? Hepatobiliary Surg Nutr 2016;5:281-9.
8. Kawaguchi Y, Fuks D, Kokudo N, Gayet B. Difficulty of laparoscopic liver resection: proposal for a new classification. Ann Surg 2018;267:13-7.
9. Kawaguchi Y, Tanaka S, Fuks D, et al. Validation and performance of three-level procedure-based classification for laparoscopic liver resection. Surg Endosc 2020;34:2056-66.
10. Strasberg SM. Nomenclature of hepatic anatomy and resections: a review of the Brisbane 2000 system. J Hepatobiliary Pancreat Surg 2005;12:351-5.
11. Tomishige H, Morise Z, Kawabe N, et al. Caudal approach to pure laparoscopic posterior sectionectomy under the laparoscopy-specific view. World J Gastrointest Surg 2013;5:173-7.
12. Wakabayashi G, Cherqui D, Geller DA, Han HS, Kaneko H, Buell JF. Laparoscopic hepatectomy is theoretically better than open hepatectomy: preparing for the 2nd International Consensus Conference on Laparoscopic Liver Resection. J Hepatobiliary Pancreat Sci 2014;21:723-31.
13. Ogiso S, Nomi T, Araki K, et al. Laparoscopy-specific surgical concepts for hepatectomy based on the laparoscopic caudal view: a key to reboot surgeons’ minds. Ann Surg Oncol 2015;22 Suppl 3:S327-33.
14. Giuliani A, Aldrighetti L, Di Benedetto F, et al. Total abdominal approach for postero-superior segments (7, 8) in laparoscopic liver surgery: a multicentric experience. Updates Surg 2015;67:169-75.
15. Ogiso S, Conrad C, Araki K, Nomi T, Anil Z, Gayet B. Laparoscopic transabdominal with transdiaphragmatic access improves resection of difficult posterosuperior liver lesions. Ann Surg 2015;262:358-65.
16. Xiao L, Xiang LJ, Li JW, Chen J, Fan YD, Zheng SG. Laparoscopic versus open liver resection for hepatocellular carcinoma in posterosuperior segments. Surg Endosc 2015;29:2994-3001.
17. Boggi U, Caniglia F, Vistoli F, Costa F, Pieroni E, Perrone VG. Laparoscopic robot-assisted resection of tumors located in posterosuperior liver segments. Updates Surg 2015;67:177-83.
18. Montalti R, Scuderi V, Patriti A, Vivarelli M, Troisi RI. Robotic versus laparoscopic resections of posterosuperior segments of the liver: a propensity score-matched comparison. Surg Endosc 2016;30:1004-13.
19. Scuderi V, Barkhatov L, Montalti R, et al. Outcome after laparoscopic and open resections of posterosuperior segments of the liver. Br J Surg 2017;104:751-9.
20. D’Hondt M, Tamby E, Boscart I, et al. Laparoscopic versus open parenchymal preserving liver resections in the posterosuperior segments: a case-matched study. Surg Endosc 2018;32:1478-85.
21. Okuno M, Goumard C, Mizuno T, et al. Operative and short-term oncologic outcomes of laparoscopic versus open liver resection for colorectal liver metastases located in the posterosuperior liver: a propensity score matching analysis. Surg Endosc 2018;32:1776-86.
22. Nota CL, Woo Y, Raoof M, et al. Robotic versus open minor liver resections of the posterosuperior segments: a multinational, propensity score-matched study. Ann Surg Oncol 2019;26:583-90.
23. Aghayan DL, Fretland ÅA, Kazaryan AM, et al. Laparoscopic versus open liver resection in the posterosuperior segments: a sub-group analysis from the OSLO-COMET randomized controlled trial. HPB (Oxford) 2019;21:1485-90.
24. Zheng H, Huang SG, Qin SM, Xiang F. Comparison of laparoscopic versus open liver resection for lesions located in posterosuperior segments: a meta-analysis of short-term and oncological outcomes. Surg Endosc 2019;33:3910-8.
25. Jang JY, Han HS, Yoon YS, et al. Three-dimensional laparoscopic anatomical segment 8 liver resection with glissonian approach. Ann Surg Oncol 2017;24:1606-9.
26. Sakai H, Hisaka T, Okuda K. Laparoscopic liver resection using the silicone band uplift technique for tumors in segments 8 and 7 (with video). J Visc Surg 2017;154:375-6.
27. Sugioka A, Kato Y, Tanahashi Y, et al. Concept of laennec’s capsule and laparoscopic segmentectomy 8. Rinsyogeka 2017;72:284-94. Available from: https://cir.nii.ac.jp/crid/1370294643800191488. [Last accessed on 3 Jan 2022]
28. Berardi G, Wakabayashi G, Igarashi K, et al. Full Laparoscopic anatomical segment 8 resection for hepatocellular carcinoma using the glissonian approach with indocyanine green dye fluorescence. Ann Surg Oncol 2019;26:2577-8.
29. Kim JH. Pure laparoscopic anatomical resection of the segment 8 dorsal area using the transparenchymal Glissonean approach (Video). Surg Oncol 2019;31:99-100.
30. Ome Y, Honda G, Doi M, Muto J, Seyama Y. Laparoscopic anatomic liver resection of segment 8 using intrahepatic glissonean approach. J Am Coll Surg 2020;230:e13-20.
31. Turco C, Lim C, Goumard C, Scatton O. Laparoscopic anatomic liver resection of segment 8 using the transfissural glissonean approach: the ton that tung technique revisited. J Am Coll Surg 2020;230:836.
32. You N, Wu K, Li J, Zheng L. Laparoscopic liver resection of segment 8 via a hepatic parenchymal transection-first approach guided by the middle hepatic vein. BMC Gastroenterol 2022;22:224.
33. Sandroussi C, Greig PD. Chapter 92. Segment-oriented anatomic liver resections. Blumgart’s Surgery of the Liver, Biliary Tract, and Pancreas. 5th ed. Elsevier Saunders; 2012.
34. Takayama T, Makuuchi M, Kogure K. Relevant hepatobiliary anatomy. Laparoscopic liver, pancreas, and biliary surgery. 1st ed. 2016. pp.148-68.
35. Wakabayashi G, Cherqui D, Geller DA, et al. The Tokyo 2020 terminology of liver anatomy and resections: updates of the Brisbane 2000 system. J Hepatobiliary Pancreat Sci 2022;29:6-15.
36. Cho A, Okazumi S, Takayama W, et al. Anatomy of the right anterosuperior area (segment 8) of the liver: evaluation with helical CT during arterial portography. Radiology 2000;214:491-5.
37. Ome Y, Honda G. Anatomic liver resection of segment 8. Japanese mastery in hepato-pancreato-biliary surgery. 1st ed. Gakken; 2021.
38. Anselmo A, Sensi B, Bacchiocchi G, Siragusa L, Tisone G. All the routes for laparoscopic liver segment VIII resection: a comprehensive review of surgical techniques. Front Oncol 2022;12:864867.
39. Efanov M, Salimgereeva D, Alikhanov R, et al. Comparison between the difficulty of laparoscopic limited liver resections of tumors located in segment 7 versus segment 8: an international multicenter propensity-score matched study. J Hepatobiliary Pancreat Sci 2022;30:177-91.
40. Ishizawa T, Gumbs AA, Kokudo N, Gayet B. Laparoscopic segmentectomy of the liver: from segment I to VIII. Ann Surg 2012;256:959-64.
41. Lee W, Han HS, Yoon YS, Cho JY, Choi Y, Shin HK. Role of intercostal trocars on laparoscopic liver resection for tumors in segments 7 and 8. J Hepatobiliary Pancreat Sci 2014;21:E65-8.
42. Inoue Y, Suzuki Y, Fujii K, et al. Laparoscopic liver resection using the lateral approach from intercostal ports in segments VI, VII, and VIII. J Gastrointest Surg 2017;21:2135-43.
43. Hirokawa F, Hayashi M, Asakuma M, Shimizu T, Inoue Y, Uchiyama K. Intercostal trocars enable easier laparoscopic resection of liver tumors in segments 7 and 8. World J Surg 2017;41:1340-6.
44. Shimada M, Matsumata T, Taketomi A, et al. A new approach for liver surgery. Transdiaphragmatic hepatectomy for cirrhotic patients with hepatocellular carcinoma. Arch Surg 1995;130:157-60.
45. Pocard M, Sauvanet A, Regimbeau JM Duwat O, Farges O, Belghiti J. Limits and benefits of exclusive transthoracic hepatectomy approach for patients with hepatocellular carcinoma. Hepatogastroenterology 2002;49:32-5.
46. Smyrniotis V, Arkadopoulos N, Theodosopoulos T, et al. Transdiaphragmatic approach facilitates resection of large (> 12 cm) liver tumors. J Hepatobiliary Pancreat Surg 2007;14:383-6.
47. Delis SG, Bakoyiannis A, Madariaga J, Tassopoulos N, Dervenis C. Transthoracic approach (TTA) for subdiaphragmatic liver metastasectomy. J Gastrointestin Liver Dis 2008;17:39-42.
48. Golse N, Ducerf C, Rode A, Gouillat C, Baulieux J, Mabrut JY. Transthoracic approach for liver tumors. J Visc Surg 2012;149:e11-22.
49. Teramoto K, Kawamura T, Takamatsu S, Noguchi N, Nakamura N, Arii S. Laparoscopic and thoracoscopic partial hepatectomy for hepatocellular carcinoma. World J Surg 2003;27:1131-6.
50. Teramoto K, Kawamura T, Takamatsu S, et al. Laparoscopic and thoracoscopic approaches for the treatment of hepatocellular carcinoma. Am J Surg 2005;189:474-8.
51. Cloyd JM, Visser BC. Video-assisted thoracoscopic transdiaphragmatic liver resection for hepatocellular carcinoma. Surg Endosc 2012;26:1772-6.
52. Aikawa M, Miyazawa M, Okamoto K, et al. Thoracoscopic hepatectomy for malignant liver tumor. Surg Endosc 2014;28:314.
53. Hallet J, Soler L, Diana M, et al. Trans-thoracic minimally invasive liver resection guided by augmented reality. J Am Coll Surg 2015;220:e55-60.
54. Yamashita S, Loyer E, Kang HC, et al. Total transthoracic approach facilitates laparoscopic hepatic resection in patients with significant prior abdominal surgery. Ann Surg Oncol 2017;24:1376-7.
55. Zhu Y, Li ZY, Wang CG, Fang ZP, Jia WD, Zhang FB. Laparoscopic combined with thoracoscopic transdiaphragmatic hepatectomy for hepatitis B-related hepatocellular carcinoma located in segment VII or VIII. Hepatobiliary Pancreat Dis Int 2020;19:291-4.
56. Qin L, Fei L, YongGang W, Bo L. Use of transthoracic transdiaphragmatic approach assisted with radiofrequency ablation for thoracoscopic hepatectomy of hepatic tumor located in segment VIII. J Gastrointest Surg 2019;23:1547-8.
Cite This Article
Export citation file: BibTeX | RIS
OAE Style
Panettieri E, Vega EA, Conrad C. Minimally invasive transthoracic resection of a segment eight liver tumor. Mini-invasive Surg 2023;7:1. http://dx.doi.org/10.20517/2574-1225.2022.79
AMA Style
Panettieri E, Vega EA, Conrad C. Minimally invasive transthoracic resection of a segment eight liver tumor. Mini-invasive Surgery. 2023; 7: 1. http://dx.doi.org/10.20517/2574-1225.2022.79
Chicago/Turabian Style
Panettieri, Elena, Eduardo A. Vega, Claudius Conrad. 2023. "Minimally invasive transthoracic resection of a segment eight liver tumor" Mini-invasive Surgery. 7: 1. http://dx.doi.org/10.20517/2574-1225.2022.79
ACS Style
Panettieri, E.; Vega EA.; Conrad C. Minimally invasive transthoracic resection of a segment eight liver tumor. Mini-invasive. Surg. 2023, 7, 1. http://dx.doi.org/10.20517/2574-1225.2022.79
About This Article
Special Issue
Copyright
Data & Comments
Data
 Cite This Article 15 clicks
Cite This Article 15 clicks












Comments
Comments must be written in English. Spam, offensive content, impersonation, and private information will not be permitted. If any comment is reported and identified as inappropriate content by OAE staff, the comment will be removed without notice. If you have any queries or need any help, please contact us at support@oaepublish.com.